When persistent leg pain, visible veins, or unexplained swelling begin to affect daily life, a targeted evaluation by a vein specialist can make the difference between long-term complications and effective, minimally invasive solutions. Clinics such as Metro Vein provide expert assessment, modern diagnostic tools, and personalized treatment plans that restore circulation, reduce symptoms, and minimize downtime. This article explains who vein specialists are, the conditions they treat, how problems are diagnosed, and the full spectrum of treatments available, so patients and practice owners alike can make informed decisions. For clinic owners or marketers in the healthcare space, understanding this clinical pathway also helps create accurate, helpful content that reaches patients seeking specialized vein care.
What is a Vein Specialist?
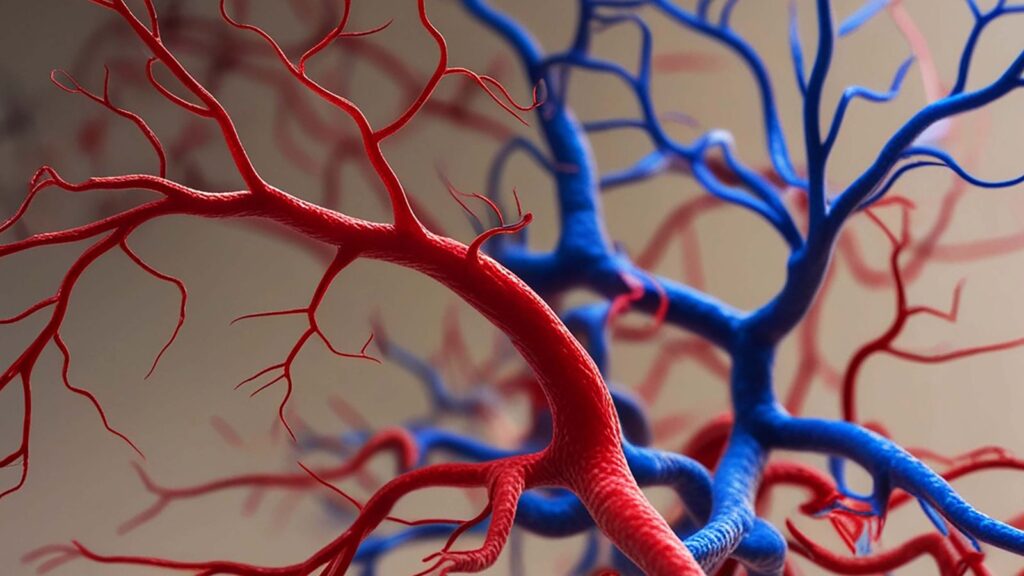
A vein specialist is a physician with focused expertise in diagnosing and treating venous disease, conditions that affect the veins rather than arteries or the heart. Rather than a single standardized title, vein specialists come from several backgrounds and often work in multidisciplinary teams to deliver comprehensive care. Patients typically consult these clinicians for issues ranging from cosmetic spider veins to serious chronic venous insufficiency.
Types of Vein Specialists (Phlebologist, Vascular Surgeon, Interventional Radiologist)
- Phlebologist: A phlebologist is a clinician who specializes specifically in vein disease. Many phlebologists are dermatologists or internists who pursued additional training in vein treatments such as sclerotherapy and endovenous procedures. They tend to focus on superficial venous issues and cosmetic concerns as well as symptomatic varicose veins.
- Vascular Surgeon: Vascular surgeons are surgeons who treat disorders of the entire vascular system (veins and arteries). They perform both open surgical procedures and endovascular interventions. When venous disease is complicated, deep vein thrombosis (DVT), venous ulcers, or recurrent varicose veins after prior procedures, a vascular surgeon often leads care.
- Interventional Radiologist: Interventional radiologists use image-guided, minimally invasive techniques to treat veins. Procedures such as venous embolization for pelvic congestion syndrome or image-guided sclerotherapy are commonly performed by these specialists. Their strength is precise, catheter-based treatment under real-time imaging.
Each specialist brings a slightly different skill set. For patients, the key is matching the clinician’s expertise to the clinical problem: for practice owners or marketers, highlighting those distinctions helps potential patients choose the right provider.
What Conditions Vein Specialists Treat
Vein specialists manage a broad spectrum of venous disorders that vary in seriousness and symptom burden. Recognizing the range helps patients know when to seek care and helps clinics prioritize the services they promote.
Common Symptoms and Risk Factors
Common symptoms prompting evaluation include:
- Aching, throbbing, or heaviness in the legs
- Visible bulging varicose veins or spider veins
- Swelling (edema), especially after prolonged standing
- Itching, skin discoloration, or persistent ulcers near the ankles
- Sudden calf pain or swelling is a possible sign of DVT
Risk factors include age, family history, pregnancy, obesity, prolonged sitting or standing, hormone therapy, and a history of blood clots. Lifestyle and occupational factors matter: someone working long-standing shifts may notice earlier progression.
Diagnostic Tests and Imaging (Venography, ABI)
Diagnosis relies on a mix of clinical exam and imaging:
- Venography: An invasive imaging test where dye is injected to map veins: used selectively when ultrasound is inconclusive or for complex cases.
- Ankle-Brachial Index (ABI): Although ABI primarily evaluates arterial disease, it’s useful when leg symptoms might be arterial rather than venous, guiding appropriate referrals.
Accurate diagnosis is critical: treating the wrong problem or a superficial issue when deep venous disease exists can lead to poor outcomes. Vein specialists interpret these tests to craft individualized treatment plans.
How Vein Specialists Diagnose Problems
A thoughtful diagnostic pathway starts with a detailed history and physical exam, then uses targeted tests. Vein specialists prioritize ruling out dangerous conditions while identifying the root cause of symptoms.
Clinical Evaluation and Medical History
During the initial visit, the specialist reviews symptoms’ onset, duration, triggers, and family history. Important details include prior clotting events, pregnancy history, previous vein procedures, medications (like blood thinners or hormone therapy), and lifestyle factors. The physical exam inspects for visible venous abnormalities, skin changes, ulcers, and measures limb circumference to assess swelling.
Treatment Options Offered by Vein Specialists
Treatment ranges from conservative measures that patients can start at home to advanced interventions. The choice depends on severity, patient goals (symptom relief vs. cosmetic improvement), and underlying anatomy.
Conservative and Preventive Measures (Compression, Lifestyle, Medication)
For many patients, conservative care reduces symptoms and complements procedural treatments:
- Compression Therapy: Graduated compression stockings remain a cornerstone for symptom control and preventing progression.
- Lifestyle Changes: Weight loss, regular exercise, limb elevation, and avoiding prolonged immobility help manage venous symptoms.
- Medication: Venoactive drugs and short-term anti-inflammatories can relieve discomfort; anticoagulation is essential for active DVT.
Conservative care is often the first step and may be the long-term strategy for milder disease.
Minimally Invasive Procedures (Sclerotherapy, Endovenous Ablation, Embolization)
Minimally invasive options have transformed vein care by reducing recovery time and complications:
- Sclerotherapy: A chemical irritant is injected into small varicose or spider veins, causing them to collapse and fade. It’s ideal for superficial, cosmetic concerns and is often performed in-office.
- Endovenous Thermal Ablation (Radiofrequency or Laser): These procedures use heat delivered inside the vein to close refluxing superficial veins like the great saphenous vein. Most patients return to normal activity within days.
- Venous Embolization: Used for pelvic congestion syndrome and certain pelvic varicosities, embolization blocks abnormal veins via catheter-delivered coils or glue.
These interventions are typically outpatient, use local anesthesia, and have durable results when applied to appropriate anatomy.
Recovery Expectations and Follow-Up Care
Recovery varies: conservative care requires ongoing adherence, while minimally invasive procedures usually involve brief downtime and compression for a few days to weeks. Follow-up imaging (often duplex ultrasound) confirms vein closure and monitors for recurrence. Vein disease can be chronic: specialists emphasize long-term surveillance and risk reduction.
When to See a Vein Specialist
Knowing when to consult a vein specialist prevents complications and improves outcomes. Timely evaluation is especially important when signs suggest acute or progressive disease.
Warning Signs that Need Prompt Evaluation
Seek immediate care if any of the following occur:
- Sudden, severe leg pain, swelling, or warmth, possible DVT
- Rapidly spreading redness or fever near a vein, possible infection
- Nonhealing leg ulcers or worsening skin changes (hyperpigmentation, eczema-like dermatitis)
- New neurologic symptoms or severe pain after a procedure
These symptoms may require urgent imaging and anticoagulation or intervention.
Routine Reasons to Seek Consultation (Cosmetic Versus Medical)
Patients commonly seek specialists for:
- Cosmetic concerns: spider veins and surface varicosities
- Chronic symptoms: aching, leg heaviness, or intermittent swelling
- Recurrence after prior vein treatments
- Preoperative evaluation of venous disease may complicate other surgeries
Clear triage between cosmetic and medical indications helps clinics set expectations and plan care pathways.
Choosing the Right Vein Specialist
Selecting a specialist involves clinical competence, clear communication, and practical considerations like cost and access. Patients and referral partners should evaluate providers on several dimensions.
Questions to Ask During Your First Visit
- What is your training and experience with this specific condition?
- Which diagnostic tests do you recommend and why?
- What are the treatment options, risks, and expected outcomes?
- Who will manage follow-up care and possible complications?
- Can you show before-and-after examples or patient outcomes?
These questions clarify expertise and set realistic expectations.
Insurance, Costs, and Coverage Considerations
Insurance coverage varies by procedure and indication. Cosmetic treatments may not be covered: medically necessary treatments (e.g., for ulcers or DVT) often are. Specialists and their administrative teams should provide transparent cost estimates, prior-authorization support, and payment options. For clinics, publishing clear guidance on coverage and typical out-of-pocket costs improves patient trust.
Finding Specialists Near You and Telehealth Options
Patients can search professional societies, hospital vascular programs, or local clinic listings. Telehealth offers an efficient first step for history-taking and triage: many specialists use virtual visits to review symptoms and plan in-person imaging if needed.
Conclusion
Vein specialists play a crucial role in diagnosing and treating a spectrum of venous disorders, from cosmetic spider veins to life-impacting chronic venous insufficiency and acute DVT. Accurate diagnosis, largely driven by duplex ultrasound, guides a treatment plan that can include conservative care, minimally invasive interventions, or surgery. For patients, early evaluation prevents progression and improves quality of life. For clinic owners and marketers, clear patient education and transparent pathways (including telehealth and insurance guidance) make care more accessible.
Healthcare practices aiming to grow their online presence, such as vascular clinics, benefit from content that mirrors this clinical clarity and answers common patient questions.
